To safely operate, an autonomous vehicle needs to be able to recognize and avoid obstacles in real time. Even a momentary lapse could lead to disastrous consequences, especially if the vehicle is a medical needle, less than a millimeter wide, navigating through the cluttered tissue of a patient’s lungs en route to a cancerous nodule.
Safely and accurately reaching a site inside living tissue is currently often challenging for physicians, especially inside complex, moving anatomy like the lung. Errors can be fatal: the failure to precisely reach a suspicious nodule in the lung can result in an inaccurate diagnosis and hence allow cancer to spread untreated. An autonomous robot has the potential to exceed the accuracy that a human operator can safely accomplish using currently available tools.
A team of researchers from the University of Utah’s John and Marcia Price College of Engineering, University of North Carolina at Chapel Hill, and Vanderbilt University have demonstrated, for the first time, a robotic needle capable of autonomously maneuvering around obstacles to a target in living tissue.
The team published this milestone result in the journal Science Robotics.
Alan Kuntz, assistant professor in the University of Utah’s Kahlert School of Computing and Robotics Center, was the study’s lead author; he began work on the robotic system as a graduate student in the lab of Ron Alterovitz, professor in the Department of Computer Science at University of North Carolina at Chapel Hill and the study’s principal investigator. They collaborated with Vanderbilt University’s Robert J. Webster III, with whom Kuntz worked as a postdoctoral researcher, as well as faculty at the University of North Carolina’s School of Medicine and Vanderbilt’s School of Medicine.
Minimally invasive medical interventions reduce pain and recovery time by threading slender, remotely-operated instruments through a natural orifice or an incision in the patient’s skin. With their small size, highly specialized probing, cutting, or cauterizing tools can also reduce trauma to the tissue surrounding the objective of the procedure, but the precision required to control such instruments is now reaching the limits of human capabilities.
Even when enhanced with mechanized assistance that allows movements measured in fractions of millimeters, human physicians must contend with unpredictable anatomical obstacles and an environment that, composed of living tissue, may be in constant motion. For particularly complicated and delicate procedures, such as biopsying a nodule in the lungs, a fully autonomous medical robot would be necessary to access the organ’s most difficult to reach areas.
“Lung cancer survival rates are much better if the disease can be diagnosed early, while nodules are small,” Kuntz says. “Current minimally-invasive biopsy methods face challenges if small nodules are far away from areas of the bronchial tree that are large enough to accommodate existing scopes and tools. Instead, our robot is able to autonomously steer through the lung tissue itself, around obstacles, to reach and home in on nodules in the furthest reaches of the lung. We believe this may open the door to earlier diagnosis and definitive treatment of lung cancer for many patients than was possible before.”
Manual versions of this procedure begin with a bronchoscope, a snake-like camera that is inserted into the patient’s lungs via their mouth or nose. While this gives a physician enough of a view to steer a manually operated needle to targets relatively close to the largest of the tree-like branches of the lungs’ airway, these branches quickly become too narrow to navigate.
“The key to our approach is the ability to accurately reach targets outside the airway,” says Webster, “Our steerable needle exits the airway and then travels to the furthest reaches of the lung, which were previously inaccessible bronchoscopically. Once we invented the steerable needle, the big challenges were how to plan needle paths, and then control the needle to travel along them. Solving these problems — along with all the real-world challenges involved in in vivo deployment — are the key results in our work.”
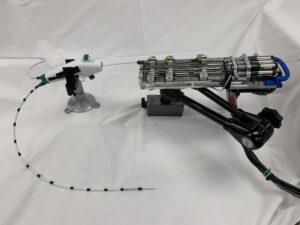
To solve this problem, the cross-disciplinary team, which includes engineers, computer scientists, and medical researchers, have developed a three-stage system capable of fully autonomous steering as it moves through the most challenging parts of the lung’s anatomy.
The first stage works like a manual bronchoscope, but can deploy a skinnier, teleoperated aiming segment deeper into the lungs. Once this second stage is correctly oriented and in position, the operator can activate the autonomous needle, which proceeds to the target on its own. Because the target nodule is often embedded deep within the lung tissue itself, this needle needs to be able to pierce into and move to the nodule while avoiding obstacles such as large blood vessels and other parts of the airway.
“This technology allows us to reach targets we can’t otherwise reach with a standard or even robotic bronchoscope,” says UNC School of Medicine Associate Professor Jason Akulian, Section Chief of Interventional Pulmonology and Pulmonary Oncology and co-author of the research team’s paper.
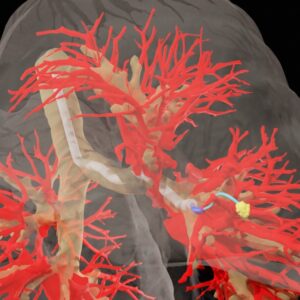
The researchers conducted their study on live porcine models, which have anatomically similar lungs to humans. By imaging the subjects’ lungs with a CT scan prior to insertion, they were able to build a 3D map for all three stages of their device’s operation, including the ultimate target for the autonomous needle.
Using magnetic coils for real-time tracking of the needle’s tip, the researchers were able to demonstrate sufficient accuracy to reach targets smaller than eight millimeters in diameter, even when the needle’s trajectory needed to be replanned to account for the movement of the subjects’ breathing.
The team plans to continue to work to bring robotic steerable needles closer to clinical use in humans by refining the system and providing further guarantees on performance in challenging cases, while also exploring new applications.
“We plan to continue creating new autonomous medical robots that combine the strengths of robotics and AI to improve medical outcomes for patients facing a variety of health challenges while providing guarantees on patient safety,” says Alterovitz.